Earlier this week the IRS announced that the Affordable Care Act Information Returns (AIR) portal will open tomorrow, Friday, January 13, 2023, at 6:00 a.m. Pacific time.
As a result of the portal opening, employers will be able to begin electronically submitting their 1094-C and 1095-C information to the IRS for the 2022 tax year. Remember, the deadline for electronically filing ACA information with the IRS for the 2022 tax year is March 31, 2023.
The portal opening this week provides employers with ample time for completing their ACA filings with the IRS, as required by the Employer Mandate.
Under the ACA’s Employer Mandate, Applicable Large Employers (ALEs), or employers with 50 or more full-time and full-time equivalent employees must:
- Offer Minimum Essential Coverage (MEC) to at least 95% of their full-time employees and their dependents whereby such coverage meets (MV), and
- Ensure that the coverage for the full-time employee is affordable based on one of the IRS-approved methods
Failing to comply with these requirements can result in ACA penalty assessments from the IRS, which the agency is currently issuing for the 2020 tax year via Letter 226J.
Below we’ve provided a checklist to help you evaluate the accuracy and completeness of your ACA reporting information for the 2022 tax year. We recommend completing the list before submitting your filings.
1. Consolidate and validate your data
Start by reviewing your HR, time & attendance, payroll, and health benefits data for each month of 2022. This step will help in ensuring an accurate and timely ACA filing with the IRS. As recently confirmed by the tax agency, good-faith transition relief for ALEs is not available after 2020 and as such makes the use of accurate data in ACA compliance filings with the IRS even more critical than ever for the 2022 tax reporting year.
2. Audit your employee classifications
Best practices encourage conducting monthly audits of your workforce data to verify accurate employment classifications, such as full-time, part-time, variable, and seasonal. The ACA’s Employer Mandate requires employers to accurately identify their full-time employees (and their dependents) and offer MEC that meets MV to at least 95% of them.
That means there’s only a 5% margin of error allowed each month. For any month that an employer strays outside of the 5% margin of error in 2022, the employer could be exposed to an annualized penalty of $2,750 multiplied by the number of full-time employees. If you have not been conducting these monthly audits, you may want to start reviewing this information before completing your filings. Doing so will give you visibility into your penalty risk exposure and allow you to plan accordingly. For more information on potential penalty exposure, get your ACA Vitals score.
3. Validate your workforce composition
It’s crucial to accurately classify employees, both at the Aggregated Employer Group level and at the level of the employer identification number (EIN). This includes knowing how many full-time and part-time employees you have and being aware of full-time employees who are not part of the Limited Non-Assessment Period.
Additionally, when using the Look-Back Measurement Method, it’s important to keep track of the numbers of “pending” and “trending” employees. Remember to also reconcile historical full-time employees who are “not in Limited Non-Assessment Period” and have not been offered health coverage.
4. Ensure ACA affordability
The ACA’s Employer Mandate also requires employers to provide coverage to full-time employees that is affordable based on one of the IRS-approved methods for calculating affordability. To meet the 2022 affordability threshold, an employee’s required contribution to the lowest cost monthly premium for Self-Only coverage providing Minimum Value should generally not exceed 9.61% of either (a) the employee’s Rate of Pay, (b) the employee’s W-2 Box 1 wages, or (c) the Federal Poverty Line threshold for a household of 1.
5. Verify data accuracy
Many of the challenges encountered on the path to ACA compliance involve data inconsistencies. Make sure your key data points are accurate, including legal name, SSN, DOB, address, employment periods, hours, wages, rate of pay, compensation type, title, employee class, location, EIN, health benefits eligibility periods, enrollment periods, and W-2 information.
Help with ACA compliance
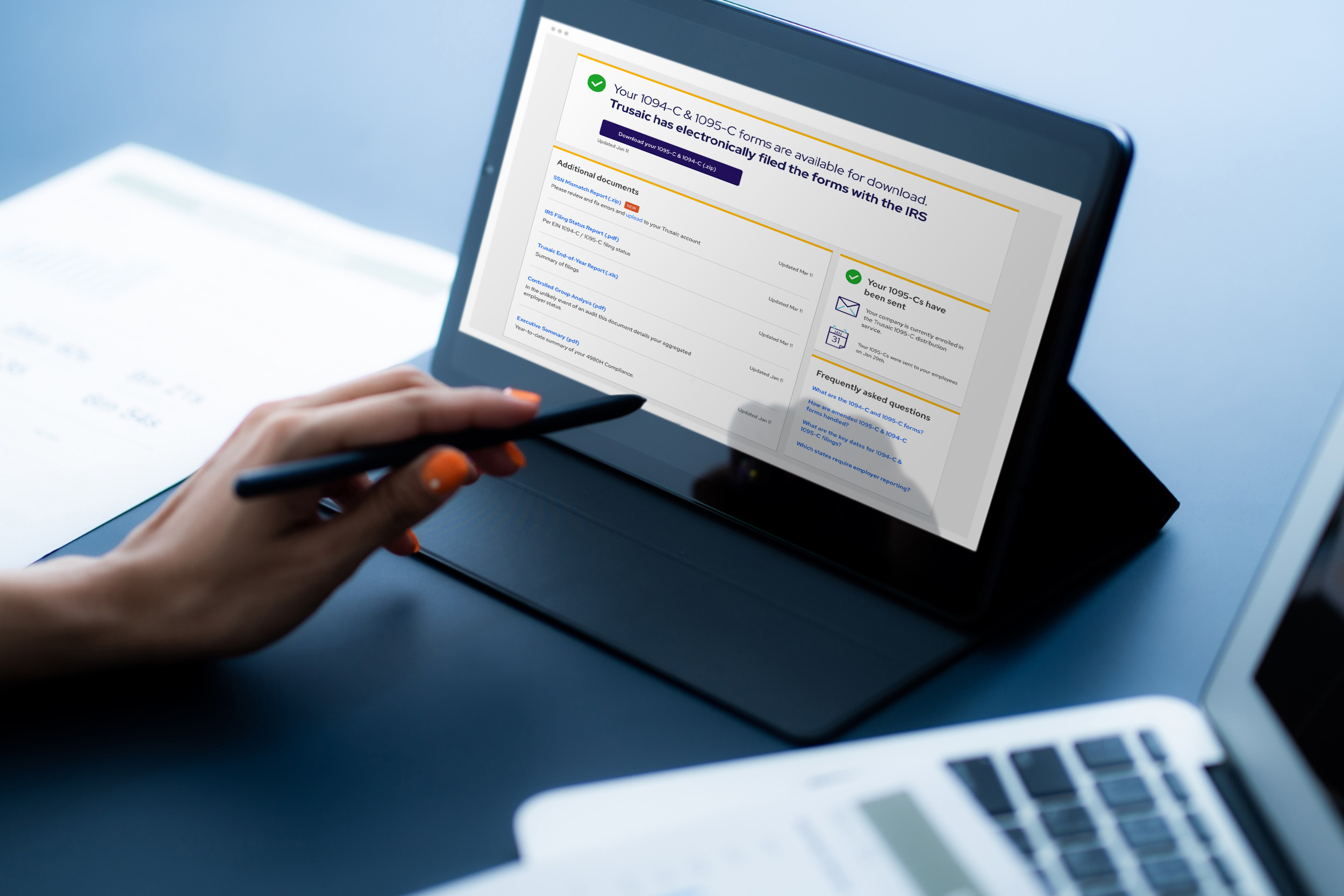
With the window for submitting ACA filings to the IRS now open, employers must act quickly if they need assistance meeting the mandated deadlines.
Trusaic’s suite of ACA services includes employee eligibility tracking, data consolidation and validation, affordability calculations, measurement method implementation, annual filing and furnishing, and IRS audit defense. We’ve helped our clients prevent over $1 billion in ACA penalties. We will waive the setup fee if you sign up for our services before January 31, 2023. Contact Trusaic to learn more.